New CU Boulder COVID-19 test
Sara Sawyer
Cheaper, faster test trades uncomfortable nose swab for spit-in-a-tube simplicity in effort to detect virus before it spreads
CU Boulder researchers have developed a rapid, portable, saliva-based COVID-19 test that can return results in 45 minutes and is easily used in community settings like schools and factories.
“We are facing a serious testing shortage in this country as more people want to get tested and diagnostics labs are overwhelmed,” said Nicholas Meyerson, a postdoctoral associate in the Sawyer Lab at the BioFrontiers Institute at CU Boulder. “We’ve developed a COVID-19 screening test that could get results to people much faster, easier and cheaper.”
The test, described in a preprint manuscript posted on the online archive MedRxiv.org, is designed for widespread screening of people who show no symptoms. Research shows people infected with the virus but with no obvious symptoms make up as many as 70% of cases and can still spread disease.
Developing ways to identify those cases early is key to reopening schools and the economy, and containing the spread of the virus, said Professor Sara Sawyer, a virologist in the Department of Molecular, Cellular and Developmental Biology who led the development of the test.
“Most tests approved to date require that the sample, even if it’s saliva, be processed using sophisticated equipment in a clinical diagnostic lab or at a doctor’s office. That can take days,” she said.
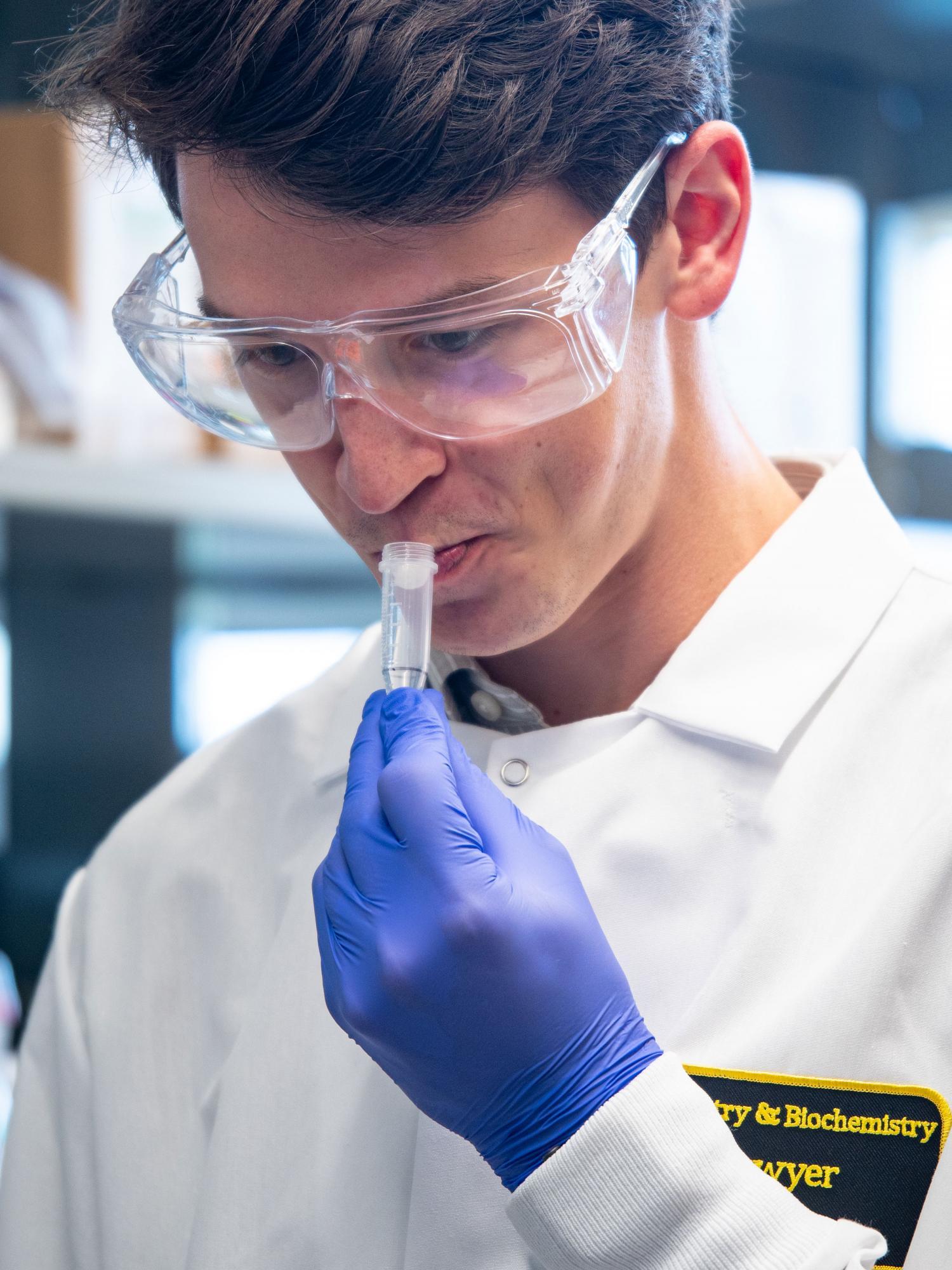
In the new test, the user drools saliva into a tube and hands it off to testing staff to process it through a simple system requiring little more than pipettes, a heat source and an enzyme mixture.
If the sample turns from pink to yellow, the test is positive. If it doesn’t, it’s negative.
Because no swabs or fancy laboratory equipment are needed, the tests are also less vulnerable to backlogs and supply chain shortages.
The test is based on a 20-year-old technology known as reverse transcription loop-mediated isothermal amplification (RT-LAMP). It has been used to screen mosquitoes for the Zika virus in remote regions of South America and in other applications.
To process, the saliva is added to three tubes, each containing a custom enzyme mixture. When heated to a certain temperature, the mixture undergoes a chemical reaction when the genetic material from SARS-CoV-2—the virus that causes COVID-19—is detected.
In one experiment described in the paper, the researchers conducted what is known as a “contrived clinical validation.” One researcher spiked 30 out of 60 saliva samples with inactivated SARS-CoV-2 in the lab, then shuffled the samples and gave them to another scientist to test with the RT-LAMP technology.
“The test predicted with 100% accuracy all of the negative samples, and 29 of 30 positive samples were predicted accurately,” Meyerson said.
While the test is slightly less sensitive than those performed in clinical labs, a separate computer modeling study found that quick turnaround is even more critical to curbing the pandemic than test sensitivity.
“Our modeling showed that whether a test is sensitive or super-sensitive is not that important,” said BioFrontiers Director Roy Parker, co-author of that paper. “What is important is frequent testing, with the test results returned as fast as possible, which identifies more infected people faster and can limit new infections.”
Those who test positive could quarantine themselves as they await confirmatory testing, Sawyer said.
The research team, with support from Venture Partners at CU Boulder, has created a spinoff company, Darwin Biosciences, to commercialize the test.
“While we are all very optimistic about a coronavirus vaccine, scientists have been working on an HIV vaccine for 30 years without success,” Sawyer said. “Meantime, the HIV pandemic showed us that pervasive testing, out in the community and not just at hospitals or urgent cares, can make a big difference.”

Principal Investigator
Sara Sawyer
Funding
National Institutes of Health
Collaboration + support
BioFrontiers Institute; Department of Molecular, Cellular and Developmental Biology; Venture Partners at CU Boulder; Darwin Biosciences

