Blog: Seniors designing tech for pediatric brain imaging
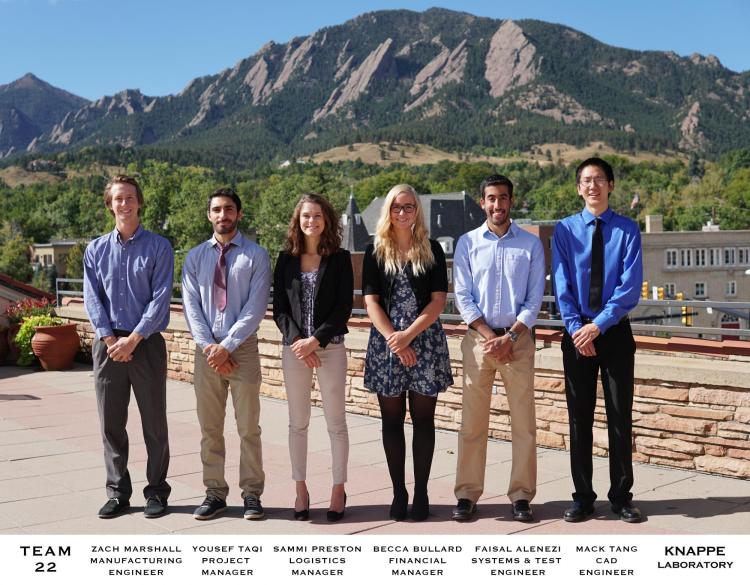
Centered around the incredible µOPM sensor technology developed by the Knappe Research Lab in the ME department at CU Boulder, a team of six undergraduate mechanical engineering seniors are designing hardware that will allow these sensors to be used for brain imaging in infants and children.
Current methods for characterizing the brain functions of an epileptic patient are very invasive and require intracranial EEG (electroencephalogram) probes to be implanted into patient's brains and monitored for days at a time. MEG (Magnetoencephalography) provides a promising solution to the current methods. This type of brain imaging allows doctors to track and observe brain activity non-invasively.
The most widely practiced method of MEG uses SQUIDs (superconducting quantum interference device). These sensors are highly sensitive to changes in magnetic fields but need to be cryogenically cooled, which prevents flexible sensor placement and results in less accurate measurements.
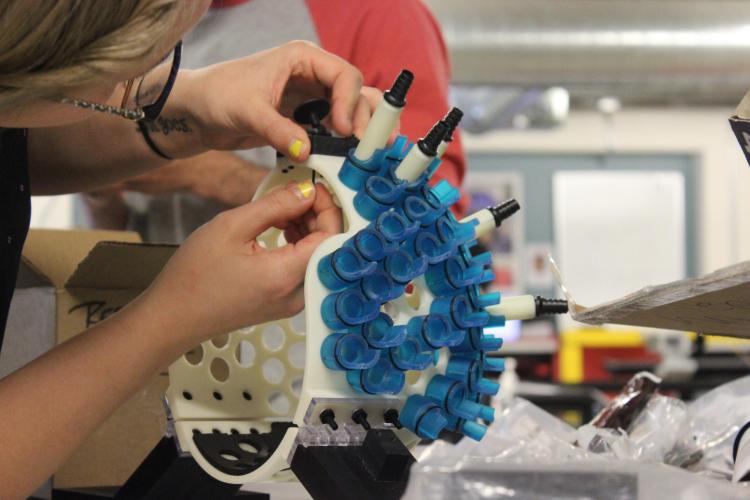
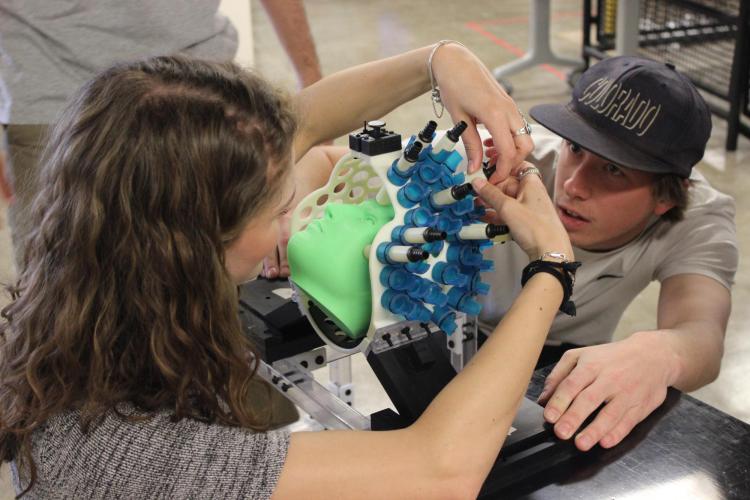
The student team was tasked with designing a Conformal MEG (cMEG) system that optimizes brain imaging in pediatric patients using Knappe's µOPMs. The cMEG system includes a helmet shell, sensor locking mechanism, safety release, and a frame.
To ensure peak performance of the µOPMs, the team designed for customizable sizing and sensor placement, minimized sensor movement, and eliminated metal contaminants. Because the system is going to be used for pediatric testing, the helmet shell accommodates for patients from six months to five years old.
One of the major design challenges is that the sensors need to be in light contact with the patient's head to minimize noise. To solve this problem, the team is developing a helmet that fits all required head sizes and provides customizable sensor placement, so technicians can fit the sensors to each patient's head.
Because the µOPM sensors are highly sensitive, vibrational and magnetic interferences need to be minimized. A locking mechanism is being developed that, when activated, ensures sensor rigidity by preventing rotational and translational movement in all directions.
Senior Design Team Members:
Feisal Alenezi
Rebecca Bullard
Zachary Marshall
Samantha Preston
Mack Tang
Yousef Taqi
To minimize magnetic interference, the materials for this project are highly restricted. No metal can be used or embedded into any of the system components. Therefore, most components are 3D printed, and all machined parts are thoroughly cleaned and tested to ensure no metal contaminants are introduced into the part during fabrication.
Because the system is meant for human use, patient safety and comfort requirements needed to be considered. The helmet shell is made of three parts: a base and two sides. This configuration ensures the patient's head is always supported by the base, while allowing the two sides to break away in case of emergency. This break away feature is controlled by a dual activation release technology that the team developed to guarantee patient safety at all times. If the patient is under distress and applies a sufficient force to the sides of the helmet, the safety release is activated, and the helmet shell breaks open. The technician is also able to manually trigger the safety release to free the patient from the helmet.
Three team members will be travelling to Boston Children’s Hospital in May to install the system and train technicians on its use.
The helmet and all its supporting features are secured to a customized frame which attaches to a patient bed at Boston Children's Hospital. There, the cMEG prototype will be used to test Knappe's µOPM sensors on pediatric patients with epilepsy. Three team members will be travelling to Boston Children’s Hospital in May to install the system and train technicians on its use.
After testing, the µOPM sensors and the cMEG system will be fabricated for clinical integration. Long term, the system could be used as a non-invasive method for diagnosing and characterizing a wide range of neurological ailments including epilepsy, autism, and traumatic brain injuries.
The team is grateful to all those that made this project possible: Svenja Knappe, Christoph Keplinger, Dr. Yoshio Okada, Design Center Colorado, ITLL, CU Mechanical Engineering Department.