New laser-based breathalyzer sniffs out COVID, other diseases in real-time
With each breath, humans exhale more than 1,000 distinct molecules, producing a unique chemical fingerprint or “breathprint” rich with clues about what’s going on inside the body.
For decades, scientists have sought to harness that information, turning to dogs, rats and even bees to literally sniff out cancer, diabetes, tuberculosis and more.
This week, scientists from CU Boulder and the National Institute of Standards and Technology (NIST) made an important leap forward in the quest to diagnose disease using exhaled breath, reporting that a new laser-based breathalyzer powered by quantum technology and artificial intelligence (AI) can detect COVID-19 in real-time with excellent accuracy.
The results were published April 5 in the Journal of Breath Research.
“Our results demonstrate the promise of breath analysis as an alternative, rapid, non-invasive test for COVID-19 and highlight its remarkable potential for diagnosing diverse conditions and disease states,” said first author Qizhong Liang, a PhD candidate in JILA and the Department of Physics at CU Boulder. JILA is a partnership between CU Boulder and NIST.
The multidisciplinary team of physicists, biochemists and biologists is now shifting its focus to a wide range of other diseases in hopes that the “frequency comb breathalyzer”—born of Nobel Prize-winning technology from CU—could revolutionize medical diagnostics.
“There is a real, foreseeable future in which you could go to the doctor and have your breath measured along with your height and weight…Or you could blow into a mouthpiece integrated into your phone and get information about your health in real-time,” said senior author Jun Ye, a JILA fellow and adjoint professor of physics. “The potential is endless.”
A COVID-born collaboration
As far back as 2008, Ye’s lab reported that a technique called frequency comb spectroscopy—essentially using laser light to distinguish one molecule from another—could potentially identify biomarkers of disease in human breath.
The technology lacked sensitivity and, more importantly, the capability to link specific molecules to disease states, so they never tested it for diagnosing illness.
But Ye’s team has since improved the sensitivity a thousandfold, enabling detection of trace molecules at the parts-per-trillion level. They’ve also harnessed the power of AI.
“Molecules increase or decrease in concentrations when associated with specific health conditions,” said Liang. “Machine learning analyzes this information, identifies patterns and develops criteria we can use to predict a diagnosis.”
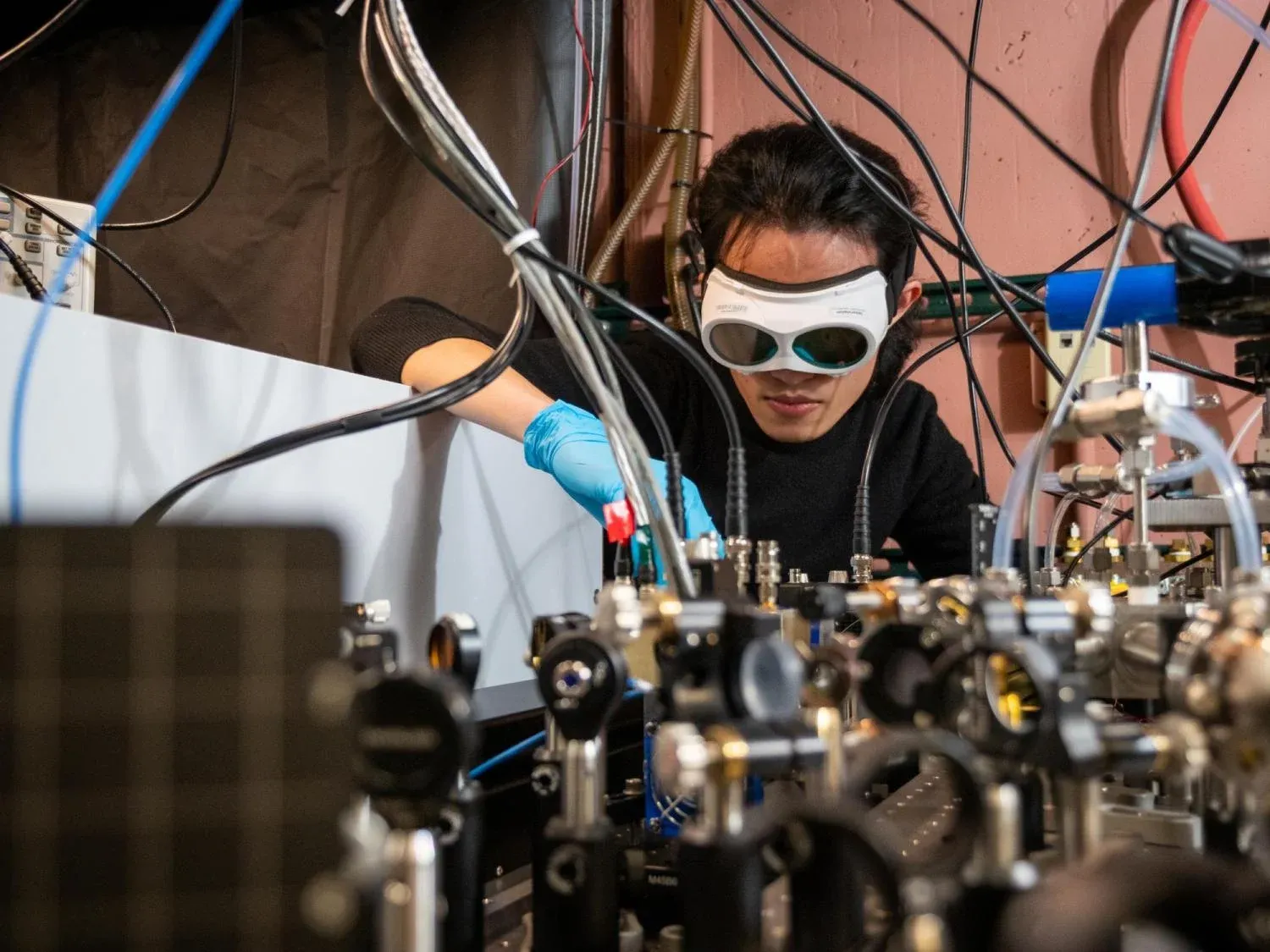
Qizhong Liang, a PhD candidate in JILA and the Department of Physics, demonstrates how the laser-based breathalyzer works, in the Ye lab at JILA. Ultimately, the system could be miniaturized for "on-the-go health monitoring." Credit: Patrick Campbell/CU Boulder
With SARS-CoV-2 ripping across the country and frustration mounting about long response times for existing tests, the time had come to test the system on people. As a physicist, Ye had never worked with human subjects, so he enlisted help from JILA physicist David Nesbitt; another JILA student Ya-Chu Chan; and CU’s BioFrontiers Institute, an interdisciplinary hub for biomedical research which was heading up the campus COVID testing program.
The National Science Foundation and the National Institutes of Health funded the research.
“This was a wonderful collaboration to bring some of the technologies that they had developed as physicists into the medical setting,” said molecular biologist Leslie Leinwand, chief scientific officer for BioFrontiers and a co-author on the study. “From the beginning, we knew there was also great potential beyond COVID.”
Non-invasive, fast, chemical-free
Between May 2021 and January 2022, the research team collected breath samples from 170 CU Boulder students who had, in the previous 48 hours, taken a polymerase chain reaction (PCR) test, either by submitting a saliva or a nasal sample. Students volunteered to be part of the study and were compensated for their time with a small gift.
Half had tested positive, half negative. (For safety reasons, participants came to an outdoor campus parking lot, blew in a sample-collection bag and left it for a lab tech waiting at a safe distance.)
Overall, the process took less than one hour from collection to result.
When compared to PCR, the gold standard COVID test, breathalyzer results matched 85% of the time. For medical diagnostics, accuracy of 80% or greater is considered “excellent.”
“We were quite pleased to see how accurate it was, especially given the lag time,” said co-author Kristen Bjorkman, director of interdisciplinary research at BioFrontiers, noting that the accuracy would likely have been higher if the breath and saliva/nasal swab samples were collected at the same time.

Qizhong Liang, a PhD candidate in JILA and the Department of Physics, poses in the lab. Credit: Patrick Campbell/CU Boulder
Unlike a nasal swab, the breathalyzer is non-invasive. And unlike a saliva sample, users are not asked to refrain from eating, drinking or smoking before using it. And unlike other tests, it doesn’t require costly chemicals to break down the sample. The new test could, conceivably, be used on individuals who are not conscious.
But there is still much to be learned, said Ye.
“With one breath, we can collect so many data points from you, but then what? We only understand how a few molecules correlate with specific conditions,” Ye said.
Building a smaller breathalyzer
Today, the “breathalyzer” consists of a complex array of lasers and mirrors about the size of a banquet table.
A breath sample is piped in through a tube as lasers fire invisible mid-infrared light at it at thousands of different frequencies. Dozens of tiny mirrors bounce the light back and forth through the molecules so many times that in the end, the light travels about 1.5 miles.
Because each kind of molecule absorbs light differently, breath samples with a different molecular make-up cast distinct shadows. The machine can distinguish between those different shadows or absorption patterns, boiling millions of data points down to—in the case of COVID—a simple positive or negative, in a matter of seconds.
Efforts are already underway to miniaturize such systems to a chip scale, allowing for what Liang imagines as “real-time, self-health monitoring on the go.” The potential does not end there.
“What if you could find a signature in breath that could detect pancreatic cancer before you were even symptomatic. That would be the home run,” said Leinwand.
Elsewhere, scientists are working to develop a Human Breath Atlas, which maps each molecule in the human exhale and correlates them with health outcomes. Liang hopes to contribute to such efforts with a larger-scale collection of breath samples.
Meanwhile, the team is collaborating with pediatric and respiratory specialists at the CU Anschutz Medical Campus to explore how the breathalyzer can not only diagnose diseases but also enable scientists to better understand them, offering hints about immune responses, nutritional deficiencies and other factors that could contribute to or exacerbate illness.
Ye and Liang continue to refine their breathalyzer to make its nose for disease even keener.
“If you think about dogs, they evolved over thousands of years to smell many different things with remarkable sensitivity,” said Ye. “We are just at the very beginning of training our laser-based nose. The more we teach it, the smarter it will be come.”
This research was funded by the Air Force Office of Scientific Research, the National Science Foundation, NIST, and the National Institutes of Health.


