CU Boulder spinoff company develops technology that could treat COVID-19 complications
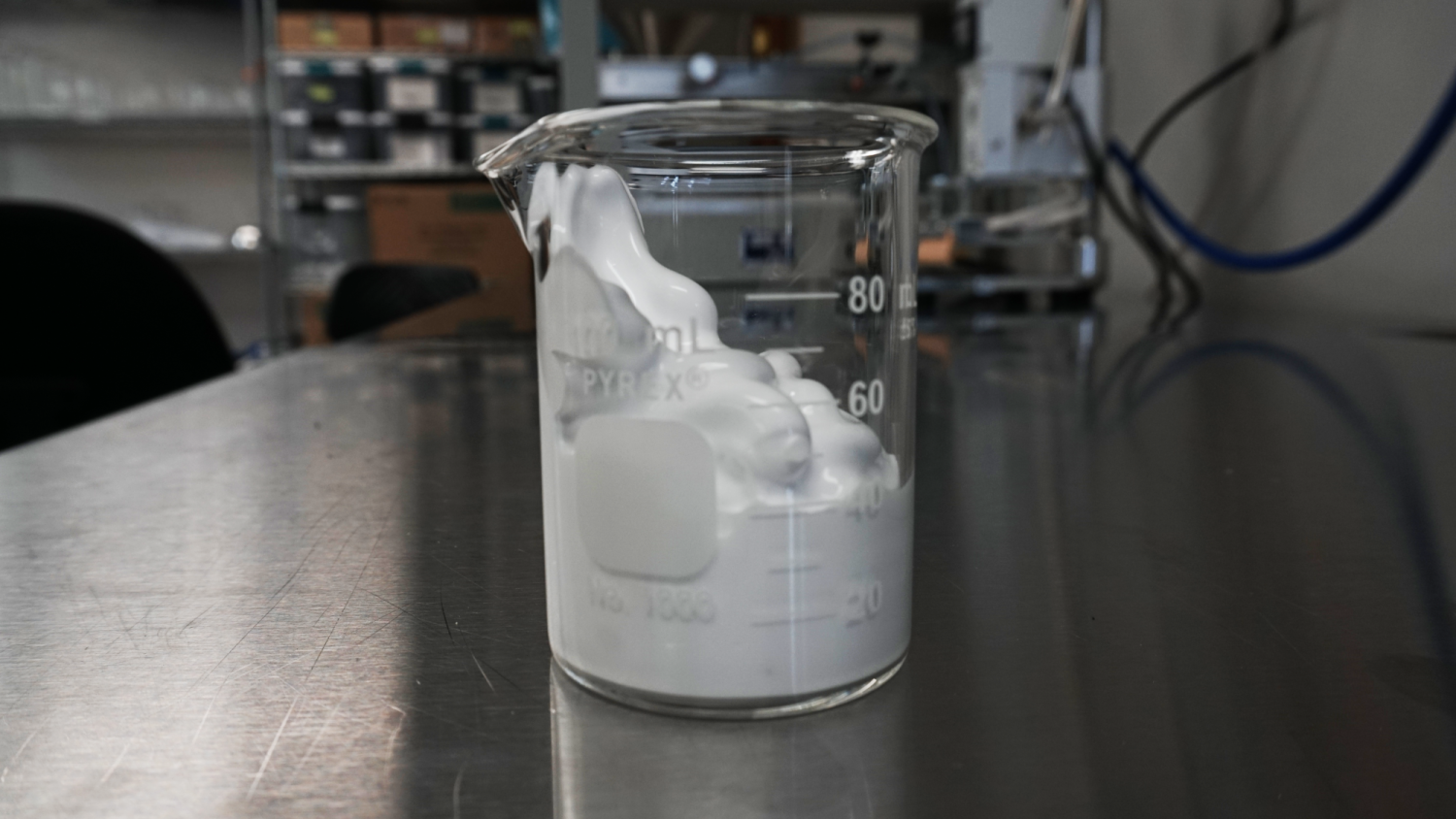
Respirogen's oxygen microbubbles take on a thick liquid form once they are fabricated. It is this liquid that would be injected into the body to oxygenate patients.
A College of Engineering and Applied Science spinoff company is on the verge of starting human trials for technology that could change the landscape for treating COVID-19 patients with one of the virus’s more severe complications.
Respirogen, a company whose research is led by Biomedical Engineering Program Director Mark Borden and founded by Borden’s former student, Paul Mountford (PhDMechEngr’15), has developed microbubbles that can deliver oxygen to the blood stream independent of the lungs.
The technology can be used to treat Acute Respiratory Distress Syndrome (ARDS) – a condition that compromises the lungs and has no cure. ARDS is caused by various illnesses or circumstances that inflame the lungs, including COVID-19, sepsis, pneumonia, near drowning or a drug reaction.
Before the COVID-19 pandemic, ARDS had a 45% mortality rate and contributed to the death of 80,000 patients in the U.S. every year. From March 2020 to October 2021, there have been roughly 700,000 deaths from COVID-mediated ARDS, according to Mountford.
Supplying oxygen is the main treatment for ARDS, and after a year when the nation experienced a shortage of mechanical ventilators, the need for novel treatments is critical. While most research focuses on anti-inflammatory agents, Respirogen is in its own space thanks to Borden’s potentially lifesaving oxygen microbubbles (OMBs).
“It would be a new pharmaceutical that could be in every hospital and every ambulance in the country,” said Borden. “It could be a gamechanger, because if you have a patient with ARDS right now, it can be a death sentence. We need to start saving lives.”
Developing the oxygen microbubbles
Professor Mark Borden, Respirogen CSO
Borden’s research began while pursuing his PhD at the University of California, Davis. He was studying microbubbles for ultrasound contrast, focusing specifically on the technology’s lipid shell.
Borden said he built a device to measure the lipid shell’s oxygen permeability, becoming the first person to do so. His research mapped the microstructure of a bubble’s surface and proved that the bubbles can be stabilized. This work propelled him to the forefront of engineering bubble technology.
“I became an expert in microbubbles by that point because most of the research prior to that had been done by industry,” Borden explained. “It was done for the purposes of minimizing costs. They were product development exercises rather than scientific studies.”
The research led to new ideas about how microbubbles could be used, including a new method to oxygenize patients suffering from ARDS.
“We know that after OMBs are delivered, a patient’s blood-oxygen levels rise and their blood-CO2 levels drop,” said Mountford. “This means that patients who may go on mechanical ventilation can be given an OMB dose and potentially kept off the ventilator. The goal of OMBs is to better ARDS patient outcomes, whether that be keeping them on mechanical support or reducing the impact mechanical ventilation has on their quality of life.”
Borden and previous colleagues thought about injecting the oxygen-filled microbubbles right into a patient’s veins, until realizing shooting 100 to 200 milliliters of oxygen into the bloodstream every minute would not be a practical option.
When Borden joined the CU Boulder faculty in 2010, he tested an idea brought to him by Mechanical Engineering PhD graduate and current University of Nebraska faculty member Benjamin Terry – to deliver OMBs through a patient’s peritoneal cavity.
Soon after, Borden approached Mountford about creating Respirogen and they brought on another ME graduate, Robby Scribner (MechEngr’10), as the company’s director of operations. The group also teamed up with CEO Bob Scribner, an experienced startup executive, and principal investigator Keely Buesing, MD, a trauma surgeon at the University of Nebraska Medical Center.
While this group found success using the peritoneal cavity during the large animal trials, they discovered this method could also be problematic. Surgery would be necessary to establish a port into the peritoneal cavity and multiple OMB injections may be needed.
After hitting that second obstacle, the Respirogen team came up with a new idea – using the colon.
The perfect solution
Mountford and Scribner handle large syringes filled with 1300ml of OMBs in the Respirogen facility.
“We have avoided the colon because everybody kind of squirms when they think about it, but on the flip side, it is the perfect solution to the problem,” said Borden. “The beautiful thing is that it works. That is what matters most.”
The notion of breathing rectally may seem peculiar, but the Respirogen team found that the hesitancy is not warranted. The colon provides easy access to the bloodstream, without surgery.
The colon is a highly vascularized tissue. One of the organ’s main functions is to remove water from stool, absorbing the water so it can be recycled back through the body. This means the colon could also absorb oxygen from OMBs and send it into the bloodstream, according to Borden.
The colon itself is easy to access as well, making multiple OMB deliveries possible. Borden explained that OMBs could be inserted rectally, flushed out with an enema and then efficiently placed back into the colon.
“There are a lot of advantages and when we redid the experiments with the colon, we were just as successful,” said Borden. “No benefits were lost by using the colon.”
The Respirogen team also pointed out that the colon is already used to administer medication to patients experiencing severe conditions. One example is when patients in hospice need pain relievers and their throats are too dry to swallow medication.
Respirogen will soon publish its OMB study involving large animals, which has been funded by the Air Force. The company has set up a first-in-human clinical trial and is looking for investors to fund it.
Treating COVID-19 complications
The COVID-19 pandemic has made treatments like Respirogen’s OMBs more important than ever, especially since there has not been a single drug approved to treat ARDS over the last 30 years, according to Borden.
Even COVID-19 patients who do not develop severe ARDS could benefit from the oxygen-filled microbubbles, Borden explained, since oxygenating the patient is a key goal in clinical management.
“We are trying to avoid mechanical ventilation, where you have a patient in an induced coma, otherwise spontaneous breathing is fighting against the machine,” said Borden. “You want to avoid that because once you start down that road, it is very hard to come off it. Supplemental oxygenation with microbubbles is such an incredibly simple solution.”
A 60ml syringe filled with OMBs shows how water within the solution can separate from the OMBs.
Throughout the pandemic, investors and the federal government have focused their coronavirus-related funding on vaccines. Mountford said that while vaccinations are one of our best lines of defense, novel therapies are needed when vaccines are not enough or if people choose not to receive their shot.
“Therapies treat symptoms from a multitude of diseases,” said Mountford. “If ARDS occurs from vaccination breakthroughs or a lack of vaccination, doctors need various ways to oxygenate patients and shed CO2. COVID-19 has not changed Respirogen's mission, but rather its ARDS patients.”
Overtime, the emphasis will likely shift from vaccines to management of the respiratory conditions that the virus leaves behind. That potential timeline would line up with Respirogen’s work.
The company’s goal is to present their human clinical data from the phase one trial sometime next year. The team wants to move into phase three human trials within five years. The next steps would be insurance reimbursement and clinical adoption.
“We do want to get this in patients’ hands as quickly as possible,” said Borden. “But we also realize that many times, medical technologies take years to be adopted. In either scenario, my lab will continue to do the research. We want to focus on doing good science and good engineering, and then let the marketplace do its job.”
Respirogen has been the only company in the oxygen microbubble space and presented their findings at the ARDS Drug Development Summit in July. Last month, a Japanese company presented a similar enteral method with liquid perfluorocarbon. Borden said the idea is such a departure from other ARDS treatments, which focus on inflammation, that it is beneficial to have more researchers studying enteral oxygenation routes.

