Lessons from the 1918/1919 Influenza Pandemic
Coronavirus interview with leading historian Susan Kingsley Kent
Interviewer: Aly Kamadia is the Editor-In-Chief of iDose
Interviewee:Dr. Susan Kingsley Kent is Arts and Sciences Professor of Distinction in the Department of History at the University of Colorado Boulder (also current Chair of the Department of Religious Studies)
Coronavirus (COVID-19) is currently intensifying its grip on the United States, United Kingdom, Canada, and many parts of the world. To the average person living in such rich countries, the global pandemic is an unprecedented event that was unimaginable.
Yet the minds of many historians have been much less shaken up: this was never a question of if, but when.
In her fantastic book titled, The Influenza Pandemic of 1918-1919: A Brief History with Documents, leading historian Susan Kingsley Kent reminded us that:
“The world seems to have dodged a bullet in 2009, but virologists expect that another influenza pandemic will emerge and sometimes worry that it will possess the capacity of its 1918 forerunner to outrun our ability to manage it.”
iDose couldn’t resist the opportunity to interview Dr. Kent. Enjoy!
Question: Dr. Kent, thank you so much for the opportunity to tap into your historical expertise.
Susan Kingsley Kent (SKK): Thank you for having me, Aly.
Q: Many experts say that the most recent point of reference for Coronavirus (COVID-19) is the 1918-1919 Influenza Pandemic (1918 Pandemic), or the so-called “Spanish Flu”. Why is that specific comparison being made?
SKK: The 1918 influenza pandemic provides a particularly apt comparison because of its global reach and the size and scope of its impact. We are also seeing certain similarities in the two events in a variety of areas. Both spread rapidly across the world. In neither instance was/is effective treatment available (at least at present). There was and is no vaccine to prevent infection and the spread of a highly contagious disease. Mortality rates appear to be similar, though these are only estimates, as we have little good data upon which to base our calculations.
Q: You note that the 1918 Pandemic killed at least 30 million people and perhaps up to 100 million – an astonishing number for a world with a population of roughly 1.5 Billion people. It killed more people than World War 1, and in the 20th century, perhaps only World War 2 exceeded its death toll. One of the things that remains tricky for many people to wrap their heads around is the question of how the virus spread so quickly in 1918. Without any significant commercial air travel and airport hubs like today, how did the virus spread to virtually every corner of the planet with such rapid speed?
The 1918 influenza pandemic provides a particularly apt comparison because of its global reach and the size and scope of its impact."
SKK: We often think of globalization as a contemporary phenomenon, but global networks and global interactions have existed for centuries. Communication and transportation were certainly slower in the early twentieth century, and the absence of air travel made them all the more so. But because the world was at war in 1918, the need to transport troops, laborers, weaponry, supplies, and foodstuffs sped up things considerably. People and goods from all over the world criss-crossed the oceans, bringing the virus to ports across the globe; once arrived onshore, it moved inland along long-standing transportation corridors.
Q: One key difference with the 1918 Pandemic and COVID-19 is that the former occurred while the World was at war. How do you think the war impacted the trajectory of virus?
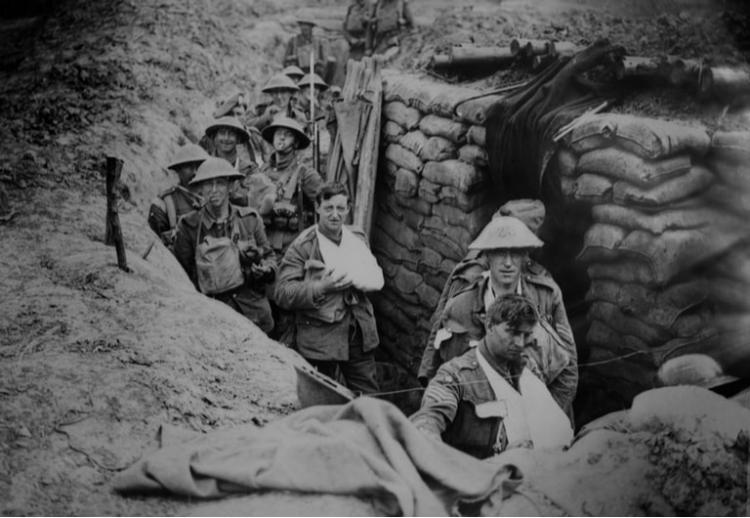
SKK: The particular configurations of the 1918 influenza virus were a product of the Great War (i.e. World War 1). The conditions of this war enabled a common and usually mild disease to mutate into a deadly strain that spread like wildfire across the globe, killing not only the weakest in the population, but the very strongest as well. Taking advantage of thousands of people congregating together in army camps and hospitals, moving constantly in and out of contact with others, and subject to conditions in the trenches that weakened immune systems, this flu took on a character unprecedented in its impact.
Flu viruses mutate regularly, but most of the viruses do not survive long enough for the changes to take effect. In ordinary conditions, a virus that mutated into a particularly deadly strain would not have sufficient hosts to sustain itself—it would kill off its hosts too quickly to be able to reproduce and pass on its characteristics.
But the conditions of warfare in 1918 ensured that sufficient hosts—young healthy men—were continuously made available, so that the virus could survive to reproduce. As soldiers fell ill, they were brought to the rear areas and replaced by others who rotated in to the camps and trenches. The camps and trenches were thus filled with men who had been infected with the virus but were not yet sick, on the one hand, and men who had not yet been exposed to the virus to whom they could transmit it, on the other.
A steady and constant supply of non-infected troops arrived to succor the virus, ensuring that its terrible virulence was not exterminated by the elimination of its hosts. Without the particular circumstances thrown up by the war, the virulent strain of influenza would not have been able to maintain its presence and take down so many victims.
The conditions of the Great War likely made it easier for the Virus to spread.
Q: Many in the general public are assuming that we’ll just have to practice self-isolation and social distancing for a short while, and this will pass. Can you tell me more about the three “waves” of the 1918/1919 Influenza? Including the idea of mutation?
SKK: The flu wreaked its havoc on military and civilian populations throughout the world in three waves. Appearing first in the American Midwest in the late winter and early spring of 1918, it spread from Camp Funston outside of Fort Riley, Kansas, to Camp Oglethorpe in Georgia, thence rapidly to Europe on board the troopships transporting American forces to the western front. An exhausted, emotionally- and physically- stressed European population proved no match for the illness, which marched through the continent en route to Asia and Africa and arrived in Australasia in July.
This first incidence caused little alarm, as it was a fairly mild strain and killed no more than the usual number of influenza victims, but it was followed by an onslaught of unprecedented force. For in mid-August, the virus mutated into a devastatingly deadly form. The second wave of the flu began to make itself felt, moving speedily along commercial and military transportation routes across the globe, leaving no one untouched. It appeared in Brest, on the northwest coast of France, around August 22. Brest served as the disembarkation port for the American Expeditionary Force, some 790,000 strong.
Some days later, the second wave appeared in Boston, the port from which a large portion of the American forces embarked en route to France. As arriving troops moved into their camps and then made their way to the front, the virus moved with them, inflicting a heavy toll in illness and deaths among the fighting forces and the hard-pressed civilian populations of Europe. From Boston, the flu travelled westward across the American continent and was carried aboard ship to the Caribbean and Central and South America.
From Russia, the flu moved into Asia; it entered India through the port of Bombay in October. It made its way to Australia, New Zealand, and the Pacific Islands by November and December.
No part of the world escaped unscathed, as this particularly lethal strain of influenza killed off millions of people.
The third wave of influenza reappeared in February 1919; less virulent than the second, it nevertheless took its toll on already-devastated populations. By the middle of 1919, the virus disappeared, probably because it had tapped into all of the human hosts available to it and burned itself out.
Q: You noted that the Influenza looks like it caused mental health issues. What sort of mental issues and to what extent?
SKK: The flu left survivors with a variety of mental symptoms. British writer Caroline Playne noted “the plague of nervous character” following the onslaught of influenza. Pronounced fatigue, lassitude, depression, sleeplessness, hallucinations, emotional lability, and even dissociation accompanied the physical debilitation of the disease.
Dr. G. Holliday wrote to the British Medical Journal on August 17, 1918, that “mental symptoms were frequent” in the cases he saw; Samuel West informed readers of The Lancet in Feb. 1, 1919, that “the depression which follows influenza is so constant that it ought to be regarded as part of the disease.” The medical correspondent for The Times, having contracted the illness himself, advised readers that “the most distressing symptom was a swift loss of mental capacity and then inability to think coherently.” “All forms of hysteria have been observed after influenza,” reported Thomson and Thomson in 1919,” such as hysterical convulsions and the so-called hystero-epilectic attacks.” “Post-influenzal neurasthenia is very familiar,” they noted, “post-influenzal psychoses” “frequently observed and reported.” They cited a study that asserted that influenza, “of all the infectious diseases . . . is the most likely to be followed by mental disorder.”
The Lancet declared in December 1918 that “the ‘higher centres’ [of the nervous system] suffer chiefly. Marked depression is common, emotional instability is often seen, and suicide is by no means rare.”
Q: My guess is that the issue of mental health during the 1918 Pandemic will surprise almost everyone reading this. In the very few instances when I’ve heard the historical flu mentioned, I have yet to hear anyone talk about mental health during the time.
You also mention that Western Scientists during the 1918 Pandemic knew very little about about the disease. How did this end up influencing public attitudes? People must have been desperate for cures when they weren’t getting any? And was there any merit in ‘Eastern’ remedies, or ‘traditional medicine’?
SKK: To their surprise, dismay, and chagrin, physicians did not know how to treat this disease. They misunderstood the etiology of the illness and prescribed often contradictory measures to treat it. Having mistaken its source as a bacillus, which, since the 1890s had been thought to be the cause of influenza, doctors resorted to treatments that could have no effect on viruses, whose role in generating influenza was only discovered in 1933. Many physicians turned to vaccines to treat their patients, but these were bound to fail in the absence of any real knowledge about what caused the disease. Ultimately, they were helpless in the face of this disease. As one American physician put it, “There was just nothing you could do.”
In a supreme irony, western physicians in China excoriated and mocked traditional Chinese medicine, little realizing that the treatments advised there included compounds that have been shown to reduce fever. Noting the effectiveness of Chinese traditional medicine in treating epidemic disease over a number of centuries, two Chinese scientists believe that the far lower rates of mortality in China were a result of peasants turning to traditional practitioners, whose successes in reducing fever by means of herbal remedies were long-standing.
In Japan, similarly, traditional treatments utilizing an oleo of dried ephedrine, peony, and ginger root proved effective in reducing fever and nasal congestion. This herbal concoction was cheap and readily available to all but the poorest Japanese, and most likely helped to control the high fever that accompanied the pneumonia that proved so deadly elsewhere. Chinese and Japanese death rates do seem to have been lower than those in other countries.
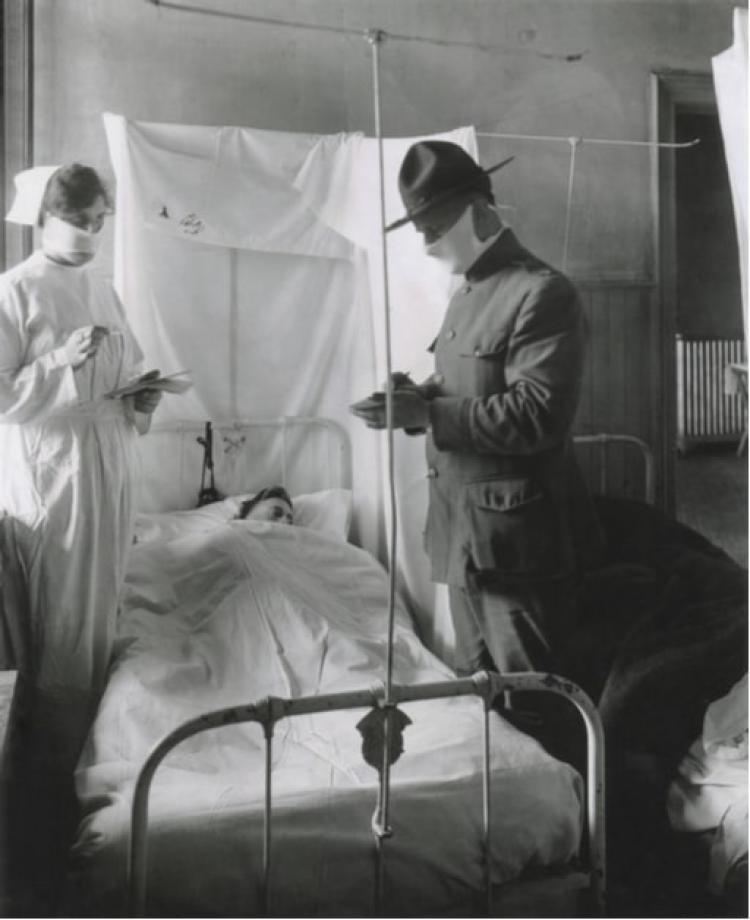
Physicians did not know how to treat the disease
Advertisements touted the benefits of alcohol, tobacco, patent medicines, or home remedies containing garlic, camphor, cinnamon, quinine, or sugar cubes soaked in kerosene. Nothing worked, though demand for any possible treatment or cure drove up the profits of those businesses offering them. Some stores lost business as customers fell sick or avoided public places, but others saw unprecedented demand for their products. One department store in Little Rock, Arkansas, noted the Arkansas Gazette on October 19, 1918, “which has a business of $15,000 daily, is not doing more than half that.” But drug stores and apothecaries couldn’t keep patent medicines in stock.
There seems to be a consensus that the 1918 Pandemic, despite its worldwide horrors, was forgotten soon enough for the most part. Why might that be?
The emotional traumas produced by the influenza pandemic of 1918-19 had a long-term impact, I would argue, on the capacity of societies to keep it within collective consciousness. The pandemic disappeared from popular memory for more than 60 years following its devastating impact. Certainly individuals wrote about their experiences, but public consciousness of this extraordinary event vanished. A few explanations suggest themselves.
First, the destruction and dislocation of the Great War itself and the subsequent global developments that flowed from it—the Russian Revolution, the Great Depression, the rise of fascism, World War II—may well have upstaged the consequences of the flu pandemic, rendering it relatively insignificant.
Perhaps equally important, the pandemic laid bare the inability of nations and peoples to prevent, control, or treat what had come to be regarded as an everyday illness. Science had failed; medicine had failed; governments had failed. Forgetting about the flu pandemic may just have appealed to publics too frightened and too freaked out to acknowledge so grand a failure on the art of institutions and agencies they had come to rely upon for protection and safety. Faced with such disturbing information, societies may have unconsciously determined that historical amnesia was the easier option.
Q: The entire Western World, including all the ‘advanced’ countries, look like they’re collectively on the way to tens of millions of people being infected. From a historical perspective, what might be some lessons that you’d highlight or reinforce to the general public on one hand, and to policy makers on the other? Does ‘history repeat itself’, to use a familiar cliché?
SKK: History doesn’t repeat itself, but it sure does offer lessons from the past that we can learn from.
In 1918, for example, the town of Gunnison, Colorado, closed itself off from all intercourse with surrounding areas. While people outside the town limits suffered grievously from influenza, Gunnison folks fared well, experiencing far fewer cases of and deaths from the disease. As is the case today, the haphazard and inconsistent responses of the individual states and municipalities across America meant that some places, like Philadelphia, incurred horrendous death rates.
If we can take anything away from the experience of 1918, it’s that people amassing in large numbers spells disaster, and that in the absence of treatment or a vaccine, social distancing and quarantine are the best means of containing pandemic illness. Indeed, the experience of pandemic influenza in 1918 compelled the creation of public health departments around the world. We should remember why that was: now, as then, an effective response must be consistent and coordinated, which requires active, clear, and coherent federal intervention.
If you enjoyed this interview, make sure to check out the important comments that Dr. Kingsley makes about the political consequences of the 1918/1919 Influenza in our bonus article
Dr. Susan Kingsley Kent is Arts and Sciences Professor of Distinction in the Department of History at the University of Colorado Boulder (also current Chair of the Department of Religious Studies)
Aly Kamadia is the Editor-In-Chief of iDose. To read selected articles by Kamadia, click here.


